Adequate Folate Levels Reduce Cardiovascular Mortality in Rheumatoid Arthritis
-
Patients with rheumatoid arthritis (RA) are at increased risk of cardiovascular mortality.
-
This study found that RA patients with low serum folate had 50% higher cardiovascular mortality risk compared to those with adequate folate.
-
Folate can lower homocysteine, an inflammatory marker related to cardiovascular disease.
This article was posted on The University of Texas Health Science Center at Houston (UTHealth) News:
Decreased folate levels in the bloodstream have been associated with an increased risk of cardiovascular mortality in patients with rheumatoid arthritis, shedding light on why those patients are more susceptible to heart and vascular disease, according to research published today in JAMA Network Open by experts at The University of Texas Health Science Center at Houston (UTHealth).
Patients with rheumatoid arthritis are 60% more likely to die from cardiovascular disease, but researchers have not been able explain why. Rheumatoid arthritis is an autoimmune disorder that causes inflammation due to immune system attacks on healthy cells. It can lead to permanent tissue and joint damage. Women are 2-3 times more likely to develop the disease.
"Our study is the first to show an association between serum folate and increased cardiovascular mortality in patients with rheumatoid arthritis," said Kalyani Sonawane, PhD, an assistant professor at UTHealth School of Public Health and the study's lead author. "It's particularly important for patients taking disease-modifying anti-rheumatic drugs to understand this increased risk."
Serum folate, more commonly known as folic acid, is a B vitamin that is essential in the creation of new cells and has a homocysteine lowering effect. Homocysteine is an amino acid found in blood, and high levels have been linked to a greater risk of developing cardiovascular disease. Individuals with rheumatoid arthritis often have an increased amount of homocysteine, an imbalance that may be due to common medications prescribed for rheumatoid arthritis, such as methotrexate, which deplete folate levels.
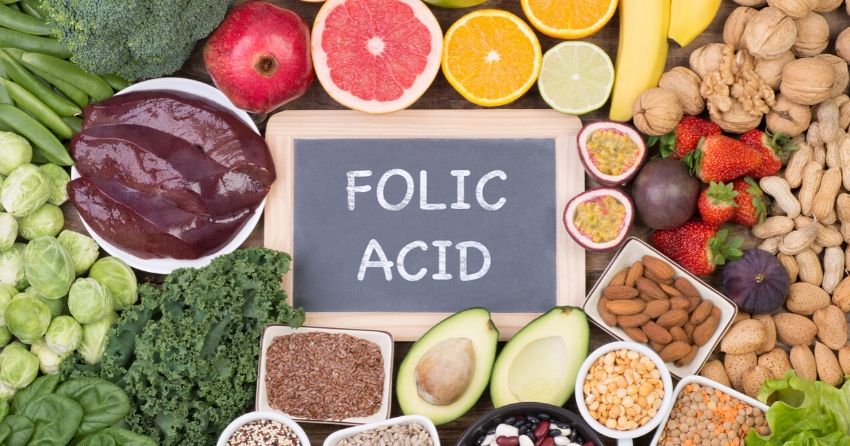
Folic acid is found in many foods such as eggs, broccoli, citrus fruits, and leafy greens. Healthy adults should consume at least 400 mcg daily, but study authors say folate-rich foods may not be enough to prevent cardiovascular disease for people with rheumatoid arthritis. Diets high in animal protein such as red meat and increased coffee consumption have been linked to higher homocysteine levels. Avoiding red meats and coffee and eating a diet rich in fruits and vegetables, in addition to taking a daily folic acid supplement, can help reduce homocysteine blood levels.
The researchers identified 683 patients with a self-reported diagnosis of rheumatoid arthritis. Participants were divided into three groups based on their measured serum folate levels: the first group (239 patients) had levels below 4.3 nanograms per milliliter; the second (234 patients) measured levels between 4.3 and 8.2 nanograms per milliliter; the third (210 patients) had levels greater than 8.2 nanograms per milliliter.
Over the course of 17 years, 258 cardiovascular deaths occurred. Serum folate level below 4.3 nanograms per milliliter was associated with 50% higher cardiovascular mortality risk in rheumatoid arthritis patients.
"Our findings suggest that serum folate level might be a useful indicator to assess cardiovascular mortality risk of a rheumatoid arthritis patient in clinical practice," said senior author Maria E. Suarez-Almazor, MD, PhD, Barnts Family Distinguished Professor at The University of Texas MD Anderson Cancer Center. "If future clinical studies validate a causal link, taking folate supplements could be an affordable way to reduce this risk in patients with rheumatoid arthritis."
The study was published in JAMA Network Open in February 2020.





