How the Gut Microbiome Contributes to Alzheimer's Disease
-
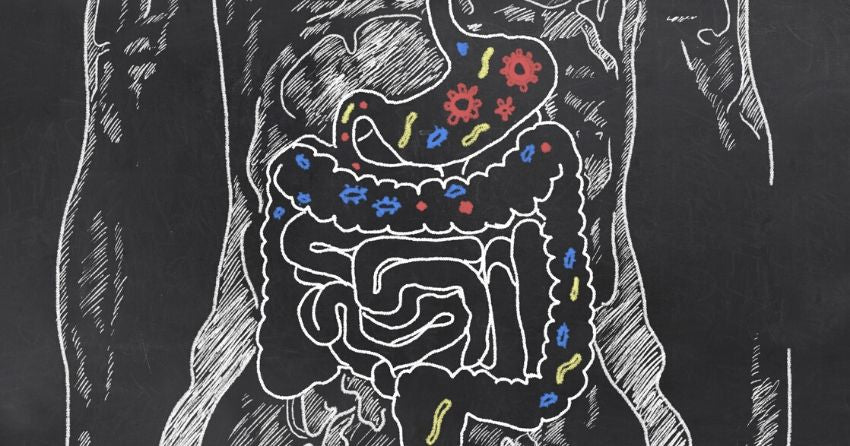
Intestinal microbes are thought to be involved in the development of Alzheimer's disease (AD), through the gut-brain-microbiota axis.
-
Gut dysbiosis leads to the release of pro-inflammatory mediators, which increase the permeability of the gut lining and the blood-brain barrier.
-
This leads to neuroinflammation and amyloid generation in the brain, which then leads to the progression of neurodegenerative diseases, like AD.
The following commentary was posted by Reason on FightAging.org:
The gut microbiome changes with age in ways that provoke chronic inflammation. Beneficial microbial populations decline in number while harmful populations expand. This is likely the result of numerous contributing factors, including dietary changes characteristic of age and the decline of the immune system, but at this point it is a challenge to pin down which of these processes are more versus less important to the overall outcome. It is well known that chronic inflammation drives a faster progression of many of the common age-related diseases, including neurodegenerative conditions. Thus it is expected to find links between the gut microbiome and conditions such as Alzheimer's disease, as is discussed here.
The study was published in Aging in March 2020:
Factors that may be involved in the development of Alzheimer's disease are thought to include lifestyle habits. Lifestyle dysregulation may not only lead to Alzheimer's disease, but also to various other health problems such as dysregulation of the gut microbiota. The composition of symbiotic microorganisms has changed dramatically throughout human history with the development of agriculture, industrialization, and globalization. It is postulated that each of these lifestyle changes resulted in a gradual disappearance of microbial diversity and an increase in their virulence, thus causing the formation of a risk path for Alzheimer's disease pathogenesis. Changes in the microbial composition throughout history suggest an escalation of the risk of Alzheimer's disease.
Recent advances in research on the etiology of Alzheimer's disease suggest that microbiota (oral, nasal, intestinal) dysbiosis during life can lead to a systemic inflammatory response and affect microglia immune response in the brain. More and more experimental and clinical data confirm the key role of intestinal dysbiosis and interaction of the intestinal microflora with the host in the development of neurodegeneration. What is more, over time, the pathological permeability of the intestinal mucosa and blood-brain barrier begins to increase and a vicious circle is formed that irreversibly destroys neurons. It is likely that the convergence of the inflammatory response from the gut along with aging and poor diet in the elderly contributes to the pathogenesis of Alzheimer's disease.
It is a promising idea for prevention or therapeutic intervention. Modulation of the gut microbiota through a personalized diet or beneficial microflora intervention like probiotics or prebiotics, changing microbiological partners and their products, including amyloid protein, can become a new treatment for Alzheimer's disease.





