Building Bone Over 40 and How Stronger Bones Lead to Longer Lives
You may think that stronger bones are solely related to things like fractures, falls, and frailty—and while this is undoubtedly true, the health and strength of our bones are also linked to longevity. But loss of bone density doesn’t only occur late in life—our bone mass is at its peak between ages 25 and 30. By our fourth decade, we experience a gradual decline in bone strength and mass—unless we proactively do something about it.
In this article, we’ll dive into the top ways you can build or maintain your bones in your 40s and beyond—and some of the research behind why stronger bones lead to longer lives.
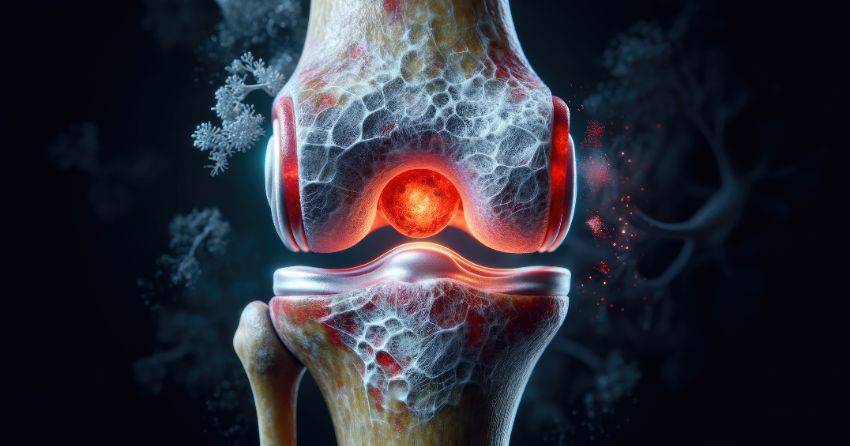
A Look at Our Aging Bones
Despite bones seeming to be static and unmoving entities, they are actually living tissue, continually being broken down and replaced by healthier bone cells. Many older adults have a declining function in these processes, making them susceptible to severe bone loss that affects their day-to-day activities and quality of life. But while you may imagine bone loss as only affecting frail and elderly adults, people in early middle age can still experience bone loss without realizing it.
Throughout life, our bodies maintain bone integrity by a process known as bone remodeling that involves cells called osteoclasts and osteoblasts. Osteoclasts work to absorb and remove older bone, allowing for the development of new bone by osteoblast cells—a process known as osteogenesis. With age, osteoblast numbers decline, leading to excessive bone removal by osteoclasts without enough new osteogenic growth to maintain bone density.
The reduced regenerative abilities of specific cells called bone marrow mesenchymal stem cells (BMSCs) may also play a role in age-related bone loss. These unique adult stem cells are found in the bone marrow and act as building blocks for skeletal tissue, as they can develop into bone-growing osteoblast cells. BMSCs have the potential for self-renewal, serving as a lifelong reservoir for creating new osteoblasts. However, the quality and quantity of available stem cells in this pool decrease with age, likely due to increased senescence—a state of irreversible cell growth arrest that renders them dysfunctional and creates inflammation in surrounding cells.
Bone cells are also susceptible to the same hallmarks of aging as other cells, including telomere shortening, DNA damage, oxidative stress, altered gene expression, and inflammatory processes, affecting osteoblasts’ ability to generate new bone.
Does Bone Health Impact Longevity?
Healthy bones are essential for quality of life, well-being, mobility, and independence as we age. More osteoporotic bone—by definition, bones that fracture easily—increases the risk of fractures and falls, which are known to increase mortality rates in older age.
Fractures—especially hip fractures—can lead to loss of mobility and other health issues that may ultimately impact life expectancy. Plus, complications arising from immobility, including being more sedentary, lead to a loss of muscle mass, which we know is vital for longevity.
In a recent study published in 2023, researchers aimed to quantify a “skeletal age” to assess fracture-related mortality. In data from over 1.6 million Danish adults, experiencing a fracture was associated with between one and seven years of life lost, with the most significant increase in mortality occurring after hip fractures. For example, a 60-year-old individual with a hip fracture was estimated to have a skeletal age of 66 for men and 65 for women, meaning their fractured bones could reduce lifespan by five to six years.
Other research has found a lower percentage of bone loss and fractures in people aged 90 and older, suggesting that better bone health plays a role in longer lifespans.
How to Build Bones Over 40
It’s not all doom and gloom when it comes to bone loss and lifespan—you can do plenty in your 40s, 50s, and beyond to ensure your bones are strong, healthy, and fracture-free.
Exercise
Many older adults—even ones who were highly active in their earlier lives—tend to cease or dwindle their exercise routines as they advance in age, whether from aches, fatigue, lack of mobility, or perceived inability, which can further the imbalance of bone remodeling.
It’s known that higher-intensity exercises, like strength, jumping, and sprint training, are beneficial to maintaining bone health and remodeling. Known as weight-bearing or bone-bearing exercise, these activities put additional stress on the bones. Although this sounds detrimental, the added stress actually helps bones stimulate calcium deposition and encourages bone-forming cells to create more, resulting in stronger and denser bones.
Both aerobic and resistance training can improve bone health. Research shows that cardio exercises like jogging can reduce bone resorption, while strength training increases bone mass. However, while walking is excellent for many aspects of health and is shown to slow down progressive loss of bone, it alone is insufficient to improve bone mass. Therefore, a combination of aerobic, high-intensity, and strength training is best for supporting strong bones with age.

Micronutrients
Calcium is the most well-known micronutrient for bone health, but several other vitamins and minerals are also involved, including magnesium, phosphorus, and vitamins D3 and K2.
- Calcium: Around 99% of the body's calcium is stored in bones and teeth, providing structure and strength. Calcium (along with phosphorus, magnesium, and collagen) participates in bone reformation and remodeling, helping to repair, maintain, and create new bone tissue.
- Vitamin D3: Vitamin D regulates the activity of phosphorus and calcium—two nutrients necessary for proper bone mineralization. With age, insufficient vitamin D can cause bone softening, loss of bone mineral density, and fractures. Research shows that each 10 ng/mL decrease in serum vitamin D levels is associated with a 33% increased risk of hip fracture in postmenopausal women.
- Vitamin K2: The bone-strengthening role of vitamin K2 was uncovered alongside the discovery of osteocalcin. This protein requires vitamins D3 and K2 to direct calcium out of the bloodstream and into the bones, where it can increase bone mineral density. Vitamin D3 and K2 work synergistically to strengthen bones. Vitamin D3's job is to direct calcium from your intestines into the bloodstream. Then, vitamin K2 finishes the job, taking calcium away from the blood (where we do not want it) and into your bones and teeth (where we want it). Without enough K2, calcium can stay in the bloodstream or calcify in the arteries and vascular tissue, causing heart issues.
- Magnesium: Like calcium, magnesium contributes to bone formation and aids in the maintenance of bone density and strength. We also need magnesium to absorb and metabolize calcium and vitamin D. Magnesium helps convert vitamin D into its active form, promoting calcium absorption in the intestines, ultimately resulting in calcium deposition into the bones.
- Phosphorus: Another mineral involved with the bones’ structure, phosphorus forms a mineral complex called hydroxyapatite that provides strength and rigidity to bones. Phosphorus is also necessary for the absorption and utilization of calcium in bones and for maintaining proper acid-base balance in the body, which is vital for bone mineralization.
Protein
While most people associate protein with muscle mass, it also plays a vital role in bone health. Research in older adults has shown that those with a higher protein intake (15% or more of total daily calories) had greater bone mineral density at the hips, lumbar spine, and whole body, with a lower risk of vertebral fracture.
Proteins—especially collagen—are essential components of the extracellular bone matrix, providing a structural framework for mineral deposition. Approximately one-third of bone mass is made up of collagen, making it vital to consume. As collagen production declines with age, supplemental collagen can help bridge this gap and provide your bones with the structural support they need. Plus, many proteins are involved with signaling pathways that regulate osteoblast and osteoclast activity and balance.
Limit Alcohol
Although you may think that alcohol only affects the liver, more and more research is accumulating to show that drinking alcohol (especially in excess) affects just about every part of our body—including our bones.
Excessive and long-term alcohol consumption interferes with bone remodeling, leading to reduced bone density. Alcohol also interferes with the ability to utilize certain vitamins and minerals essential for bone health, including vitamin D and magnesium. Plus, alcohol can disrupt estrogen levels, which can contribute to bone loss and reduced bone density.
In a meta-analysis with over 46,000 people, there was a 33% higher risk of hip fractures seen in those having three alcoholic drinks per day and a 59% increased risk in those imbibing four or more daily drinks. However, there was no effect with moderate drinking—in fact, having one daily drink was correlated with higher hip bone mineral density than people who did not drink at all.
Overall, maintaining a healthy lifestyle with a micronutrient-rich diet (especially calcium, magnesium, phosphorus, and vitamins D3 and K2), regular aerobic and resistance exercise, adequate protein intake, and low alcohol consumption can help preserve bone health with age.
References:
Benedetti MG, Furlini G, Zati A, Letizia Mauro G. Biomed Res Int. 2018;2018:4840531. Published 2018 Dec 23.
Boskey AL, Coleman R. J Dent Res. 2010;89(12):1333-1348.
Cauley JA, Lacroix AZ, Wu L, et al. Ann Intern Med. 2008;149(4):242-250.
Dayer SR, Mears SC, Pangle AK, Mendiratta P, Wei JY, Azhar G. Geriatr Orthop Surg Rehabil. 2021;12:21514593211036231. Published 2021 Aug 3.
Godos J, Giampieri F, Chisari E, et al. Int J Environ Res Public Health. 2022;19(3):1515. Published 2022 Jan 28.
Halder M, Petsophonsakul P, Akbulut AC, et al. Int J Mol Sci. 2019;20(4):896. Published 2019 Feb 19.
Sampson HW. Alcohol Health Res World. 1998;22(3):190-194.
Suominen TH, Alén M, Törmäkangas T, et al. JBMR Plus. 2021;5(7):e10513. Published 2021 May 24.
Tran T, Ho-Le T, Bliuc D, et al. Elife. 2023;12:e83888. Published 2023 May 16.
Weaver AA, Tooze JA, Cauley JA, et al. J Gerontol A Biol Sci Med Sci. 2021;76(12):2213-2222.





